Yalda Afshar was about two months pregnant when reports of COVID-19 began to emerge in the United States in February last year. As an obstetrician managing high-risk pregnancies at the University of California, Los Angeles, Afshar knew that respiratory viruses are especially dangerous to pregnant women. There was very little data on the effects of the SARS-CoV-2 virus and, as cases racked up, she felt like she was flying blind, both while advising her patients and in navigating her own worries about contracting the virus and passing it on to her baby and family. But her situation also brought her closer to the women she was treating. “I had this sense of solidarity that I’ve not felt before,” she says. “It was an inspiration to just work harder and try to get answers faster.”
Afshar launched one of the first registries in the United States to track women who had tested positive for the virus during their pregnancy, working with colleagues from across the country to recruit and follow participants. More than a dozen similar projects launched over the course of 2020.
Now, more than a year into the pandemic, research from groups around the world has shown that pregnant women with COVID-19 are at higher risk of hospitalization and severe disease than are women of the same age who are not pregnant. The rates of severe illness and death are also higher in pregnant women from certain minority racial and ethnic groups than in those in non-minority groups, mirroring the situation in the wider population.
The good news is that babies are mostly spared a severe respiratory infection, and do not often get sick. Samples from the placenta, the umbilical cord and blood from mothers and infants indicate that the virus rarely crosses from mother to fetus. However, some preliminary data suggest that infection with the virus can damage the placenta, possibly causing injury to the baby.
Many questions remain. Researchers want to know how widespread COVID-19 infection is among pregnant women overall, because the majority of the data are collected from women who end up in hospital for any reason during their pregnancy. They are also studying whether women are more vulnerable to getting a viral infection — or to its repercussions — in any particular phase of pregnancy or during post-partum recovery.
In particular, a data void gapes around vaccination safety. Following established norms, none of the major vaccine makers enrolled pregnant women in its first trials, although some current and planned trials now include them. As health systems around the world began to churn out shots, regulators have offered conflicting or vague recommendations about whether pregnant women should be offered the jab. In January, the World Health Organization (WHO) recommended that the messenger RNA vaccines made by Moderna and Pfizer/BioNTech be offered only to pregnant women at highest risk — those working in frontline positions or with existing health conditions — and only after consultation with their physician. It later added clarifying language that said the vaccines posed no known specific risks in pregnancy. A WHO spokesperson told Nature that, because of the lack of data, the agency “could not provide a broad recommendation for vaccination of pregnant women”.
Overwhelmingly, physicians contacted by Nature say they would recommend that pregnant women be offered the vaccine after medical consultation. “Given what we know about the increased risk of hospitalization, mortality, preterm birth — for me, it’s a no-brainer,” says Kristina Adams Waldorf, an obstetrician and a researcher at the University of Washington in Seattle.
Prenatal risks
It’s no surprise that respiratory viruses pose a threat to pregnant women, whose lungs are already working harder than usual. As the uterus grows it pushes up against the diaphragm, reducing lung capacity and taxing an oxygen supply divided between mother and fetus. On top of that, pregnancy dials down the immune system so as not to harm the baby. That makes women more susceptible to complications from infection. Take influenza: pregnant women who catch it are at higher risk of hospitalization compared with women who are not pregnant1. Pregnant women who caught the H1N1 flu during the 2009–10 pandemic were at higher risk of preterm delivery and stillbirth2.
So obstetricians worldwide watched with growing alarm early last year as SARS-CoV-2 infections picked up globally, worried about how it would affect their dual charges: mother and fetus.
The earliest data from China indicated that pregnant women didn’t fare much worse than non-pregnant women of the same age3. But doctors were sceptical. “That didn’t really resonate that well with most maternal–fetal medicine physicians,” says Andrea Edlow, an obstetrician at the Vincent Center for Reproductive Biology at Massachusetts General Hospital in Boston. Besides, she says, everybody saw the signs in their patients: “Pregnant women were getting sicker than other women.”
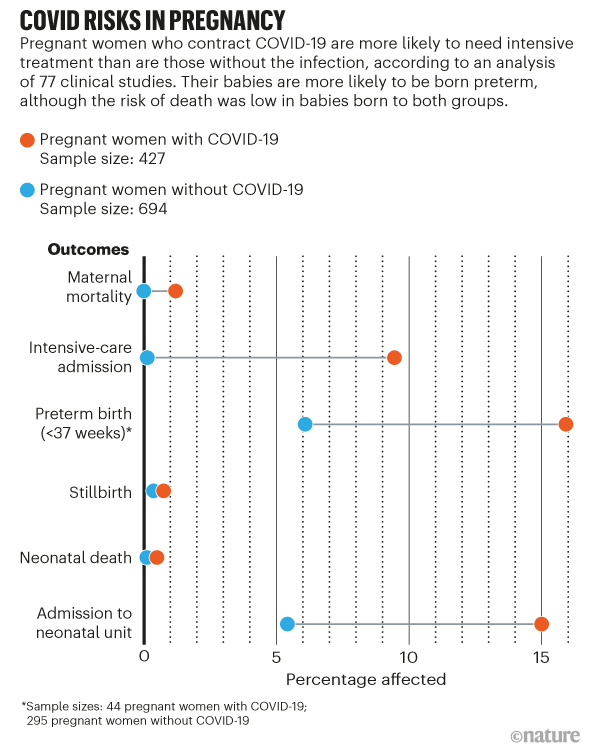
A volley of reports from around the globe began filling in the picture. An analysis of 77 cohort studies published last September4 made clear that pregnant women are a high-risk group. The review included data from more than 11,400 women with confirmed or suspected COVID-19 and who were hospitalized during their pregnancy for any reason. The odds of pregnant women with a COVID-19 diagnosis being admitted to the intensive-care unit (ICU) were 62% higher than for non-pregnant women of reproductive age, and the odds of needing invasive ventilation were 88% higher. A study5 by the US Centers for Disease Control and Prevention (CDC) echoed these findings. The study included more than 400,000 women with a positive test and symptoms of COVID-19, of whom 23,434 were pregnant, and found similar increases in the odds of ICU admission and invasive ventilation in pregnant women (see ‘COVID risks in pregnancy’).
Health-care workers should be made aware that pregnant women are less likely than non-pregnant women to show symptoms of COVID-19, says Shakila Thangaratinam, a maternal and perinatal health researcher at the University of Birmingham, UK, who led the analysis4 of the 77 studies. But she acknowledged that the sample was restricted by including only women who were hospitalized for some reason, and that this could hide the scale of the problem. “I think we need to systematically start getting information on what’s happening in the community,” she says.
Pregnant women with COVID-19 had higher rates of preterm delivery than did those without the disease, according to data from two registries that tracked more than 4,000 women with confirmed or suspected COVID-19 in the United States and the United Kingdom6. Twelve per cent of participants in the UK registry delivered before 37 weeks, compared with the rate for 2020 of 7.5% across England and Wales; in the United States, 15.7% of women with COVID-19 experienced preterm birth (the expected national rate is 10%). According to Thangaratinam’s analysis4, pregnant women with COVID-19 had three times the odds of delivering preterm compared with those without the disease.
Pregnant people from minority racial or ethnic groups seem to experience the same disparities that researchers find in COVID-19 outcomes in the wider population. “We’re seeing the exact same path,” says Monica McLemore, who studies reproductive justice at the University of California, San Francisco. To learn more, Afshar is collaborating with McLemore and others who build community participation into their studies — their registry of more than 1,300 people is 10% Black and 36% Hispanic or Latina because the group actively recruits a diverse group of patients. The cohort also includes transgender people.
Multiple studies are converging on other risk factors that worsen COVID-19 in pregnancy, including obesity, high blood pressure and gestational diabetes4. But more data are needed to quantify the part each factor plays, Thangaratinam says.
From mum to baby
If a mother contracts COVID-19, will her baby be affected? Preterm birth can lead to health issues in later life. But most preterm deliveries in women with COVID-19 occur in the last three months of pregnancy, when the fetus has the best odds of healthy development.
Reassuringly, COVID-19 has so far not been linked to a clear increase in rates of stillbirth or stalled fetal growth. “We can be relatively reassuring, because if we’re worried about stillbirth or growth restriction, that is not any more likely,” says Christoph Lees, an obstetrician at Imperial College London, who was part of the team that compared registry data for 4,000 women in the United States and the United Kingdom.
One big unknown early in the pandemic was whether SARS-CoV-2 could transmit from mother to baby. Edlow, keen to find out, pivoted her team from studies of maternal obesity in mice to building a registry of pregnant patients and a repository for biological samples. As non-essential laboratories around them closed, other medical researchers donated equipment and reagents, and Edlow’s team began collecting and studying maternal plasma, cord plasma and placentae.
Studies published from her group last December7 joined a chorus of data that showed that this ‘vertical transmission’ was rare. In 62 pregnant women who tested positive for SARS-CoV-2 by way of a nose or throat swab, Edlow’s team found no evidence of virus in the blood or cord blood, and none of the 48 babies that were swabbed tested positive for the virus at birth. “It’s a lucky asset of SARS-CoV-2 that we don’t get neonates getting really sick and dying,” Edlow says.
Afshar’s team also found that babies born to infected mothers generally fared well. In a study8 that compared 179 babies born to women who had tested positive for SARS-CoV-2 with 84 born to mothers who tested negative, most babies were healthy at birth and for 6–8 weeks after.
The question of whether a mother’s immunity transfers to her baby is a little more complicated. Edlow’s team and others have found antibodies to SARS-CoV-2 in the umbilical-cord blood of women who had been infected9,10, but it is not yet clear how much protection those levels confer on the fetus, Edlow says.
Severe viral infections in mothers have been linked to an increased chance of depression and autism spectrum disorder in their children11, and researchers wondered whether SARS-CoV-2 could also have this effect. There is no evidence yet that SARS-CoV-2 infection in mothers can affect their babies in this way, and any such links could take years to establish, but some researchers are watching their cohorts for any delays to neurological development; Afshar’s team will be tracking babies in their first year following birth.
In rare cases, the placenta can be a key player in disease, says David Baud, an obstetrician at the University of Lausanne in Switzerland who is studying a group of 1,700 pregnant women from across the world, using the architecture of a registry his team had developed to study the Zika virus in 2009.
Baud’s unpublished data suggest that in a small number of cases of COVID-19 in pregnant women, an inflammatory response — the body’s defence against the virus — damages the placental tissue in the same way as lung tissue can be ravaged. In three cases, he observed, babies whose mothers showed these placental changes were born with brain damage.
Vaccine data void
All of this convinces most physicians that pregnant women must be prioritized for COVID-19 vaccines. But because the early vaccine trials excluded pregnant women, there are unanswered questions about the safety of vaccines in this group. “I think that it was a huge mistake to not include them, because now essentially everyone is a guinea pig,” says Adams Waldorf.
Regulators have taken different paths, leaving many pregnant women to make the decision themselves. Both the CDC and the UK Joint Committee on Vaccination and Immunization recommend that pregnant women at high risk for the disease — those with an underlying condition or frontline workers — should decide with a physician whether to get a jab. The Swiss government did not initially prioritize pregnant women as vaccine roll-outs began, citing a lack of data. Baud disagrees with that decision, arguing that the risk the disease poses to pregnant people is higher, and that the biology of an mRNA vaccine poses them no specific threat. “It’s very, very, very unlikely that this vaccine will induce any problem to the pregnant patient or the fetus.” The Swiss Federal Office of Public Health now suggests that pregnant women with certain chronic illnesses consider having the vaccine.
In the United States, the Food and Drug Administration and the CDC are both monitoring the effects of vaccination in pregnant women. A team at the University of Washington set up a survey for women who are pregnant, lactating or planning a pregnancy and who had received the vaccine, and had collected 12,000 responses by the end of January. US chief medical adviser Anthony Fauci said in February that 20,000 women had received the Pfizer/BioNTech or Moderna vaccines, and agencies had found “no red flags”. And nearly a year after phase I trials of COVID-19 vaccines began in people, Pfizer has begun a trial in pregnant women.
Researchers and advocacy groups want to use the COVID-19 example to change the standards of future clinical trials, and include pregnant women from the start. The leaders of the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland, part of the US National Institutes of Health, argued12 in February that “pregnant and lactating persons should not be protected from participating in research, but rather should be protected through research”.
The concern that this group will be forgotten is what motivated Afshar to kick-start her collaboration in the first place. “Pregnant people are seriously marginalized from studies. And if we’re not doing the research to answer these questions, no one else is.”
"What" - Google News
March 09, 2021 at 07:27PM
https://ift.tt/3bqF29r
Pregnancy and COVID: what the data say - Nature.com
"What" - Google News
https://ift.tt/3aVokM1
https://ift.tt/2Wij67R
Bagikan Berita Ini

















0 Response to "Pregnancy and COVID: what the data say - Nature.com"
Post a Comment